CORNEAL TRANSPLANT FOR KERATOCONUS: PENETRATING OR LAMELLAR KERATOPLASTY
In about 24% of cases, Keratoconus progressively evolves until it reaches a point where a corneal transplant must be performed. Keratoconus is the main cause for corneal transplantation in developed countries.
When is it necessary to perform a corneal transplant?
This surgery is necessary when the cornea has become excessively thin or when central corneal scars have appeared that interfere with eyesight. In these cases corneal transplant surgery can be performed to improve vision.
The two types of Corneal transplant surgery performed are perforating and lamellar keratoplasty.
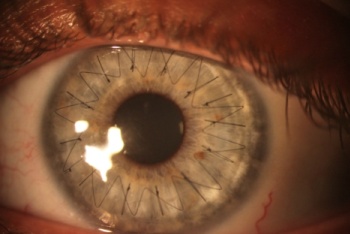
The perforating transplant completely removes the central part of the cornea and substitutes it with a new cornea of a donor.
85-90% of perforating cornea transplants are totally successful. However, about 10-15% of those operated experience either acute or chronic rejection.
Rejection is caused by the antibodies of the patient, which consider the cells of the donated cornea as extraneous and consequently react immunologically towards them, as they would do with bacteria or virus.
The rejection can be either acute or chronic, which means that it can occur either soon after the surgery, or even after many months or years. Patients will most likely need contact lenses after a transplant in order to obtain satisfactory eyesight. 80% of those operated have 5/10 vision thanks to the use of contact lenses.
5% of those operated undergo acute rejection and must repeat the operation, hoping to achieve better results. All those who experience rejection of the cornea transplant have a much higher chance of a new rejection.
Another 5-7% of cornea transplant patients undergo chronic rejection of the transplant itself with acute crisis which can be partially kept under control through specific anti-rejection medication.
Precise guidelines are followed regarding eligibility of the donor corneal tissue for corneal transplantation, however, a number of factors may affect the quality of the cornea, often the transplanted cornea often does not have the same lifespan of the original cornea.
The donated cornea gets “old” quickly for a number of reasons, which are mainly the following:
1) The length of time between the death of the donor and corneal donation is extremely important, if this interval is excessive, the cornea may be damaged.
2) The conservative liquid in which the corneas of the donor are kept after the donation is also very important, this liquid contains nutritious substances for the cornea and preservatives. Preservatives are necessary and prevent bacteria and fungus from growing into the liquid itself, but over a long period of conservation they may diminish the quality of the cornea.
3) The age of the donor may determine the quality of the cornea. For the above reasons the donated cornea has a shorter life than the original one.
When lamellar keratoplasty is performed, only part of the thickness of the cornea is removed, leaving the deepest layer intact. Consequently, risks of rejection are reduced, but other problems such as low visual quality are more likely to arise.
The above problems of keratoplasty procedures (penetrating or lamellar) explain why it is important to consider a corneal transplant only as a last resort in the treatment of keratoconus. In fact, the modern approach to keratoconus treatment is conservative, and corneal transplantation is performed only in keratoconus patients in such an advanced stage as to have no other treatment option.
Dr. Abbondanza has been studying this pathology for over 30 years and, during his career, has become one of the leading experts on keratoconus and keratoconus conservative surgery, having been the first in Italy to use the Corneal Collagen Cross-linking (2005) and having conceived himself a microsurgical technique to avoid corneal transplantation, the Mini Asymmetric Radial Keratotomy (MARK) in 1993. Thanks to these and other techniques, the need for corneal transplants keeps decreasing continuously.
.
Go to Keratoconus Conservative Surgery
.
